SEATTLE — Research at the University of Washington Medical School is finding fascinating answers to our questions about SARS-CoV-2, the virus and its variants that cause COVID-19.
One of the reasons why the omicron variant may be less lethal is demonstrated when comparing two petri dishes taken from experiments performed at UW Medicine.

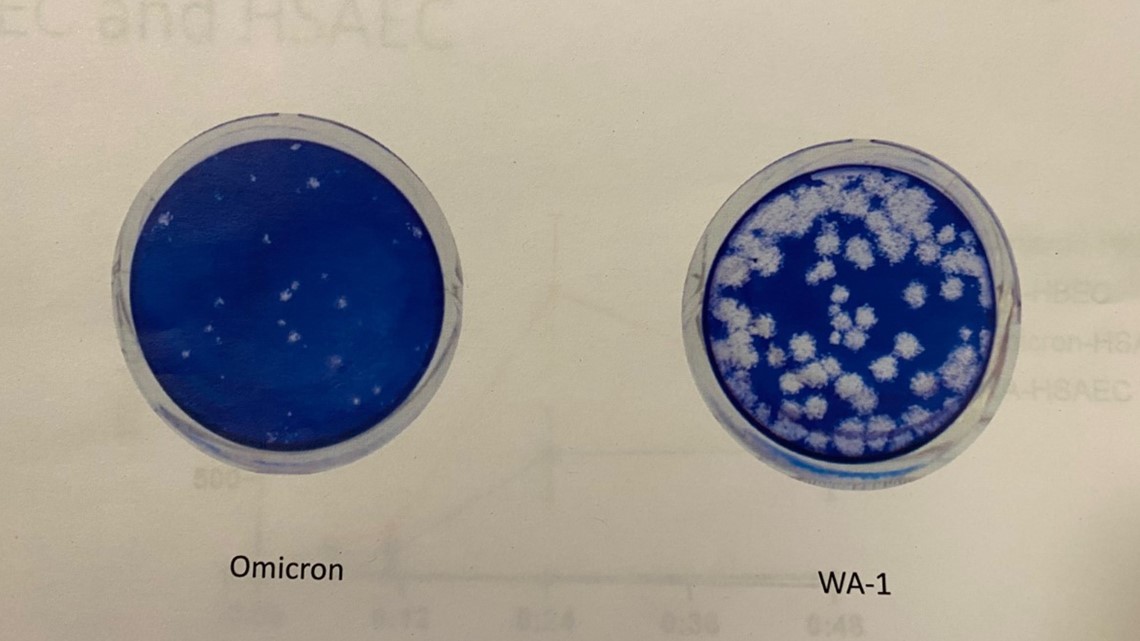
In the image above, the blue color is a carpet of stained lung cells. The one that’s nearly 100% blue shows that all but a few lung cells were able to fend off the omicron variant. The dish with lots of white is the original strain of the virus that showed up in Washington state in early 2020, devastated lung cells.
“If this were your lungs, they would be relatively protected against omicron,” said Dr. Michael Gale of that bluer dish.
Gale heads the Center for Innate Immunity and Immune Disease at UW Medicine.
“Delta looks like this also,” Gale said, pointing to the dish with lots of white plaques, as they are known.
Though lungs do well against omicron, cells in the nose do not, which is believed to make omicron so much more infectious as the disease is concentrated in the head, Gale said.
His lab at the University of Washington is trying figure out what causes the lung cells to be resistant and have innate immunity against omicron to develop a medicine that can make the nose cells more resilient to the virus and less infectious. The lab is studying more than 100 samples of live omicron viruses. Most of those samples were collected in Washington state and are compared to each other and against strains of omicron from the East Coast to South Africa.
The good news is, while the variations between different samples of omicron has changed from sample to sample, the change is fairly small, from around 1-5% different, meaning omicron is staying in its lane.
“It shows it hasn’t made any major changes that would render different clinical outcomes,” Gale said.
This lab has also studied flu. Gale believes as COVID-19 becomes endemic, meaning it will not go away entirely, the world could see the post-pandemic phase unfolding more like the flu - requiring an annual vaccine targeted to the whatever variant is making the rounds.
“I think this could be the future for us - that epidemiological surveillance globally, what type of strains are circulating - that data would be provided to the vaccine manufacturers and they would manufacture a yearly-specific vaccine like the flu,” Gale said.
To make it work though, more people need to get vaccinated he said.
When asked if omicron will eventually lead us to heard immunity: “I think we can get there faster with vaccination," he said.
Without higher vaccination rates, “It’s hard to put a number on it, but I would guess two more years of this. Is that what people really want to endure—two more years of wearing a mask and the spread of infection?"